This Is What an Adult Brain with ADHD Looks Like
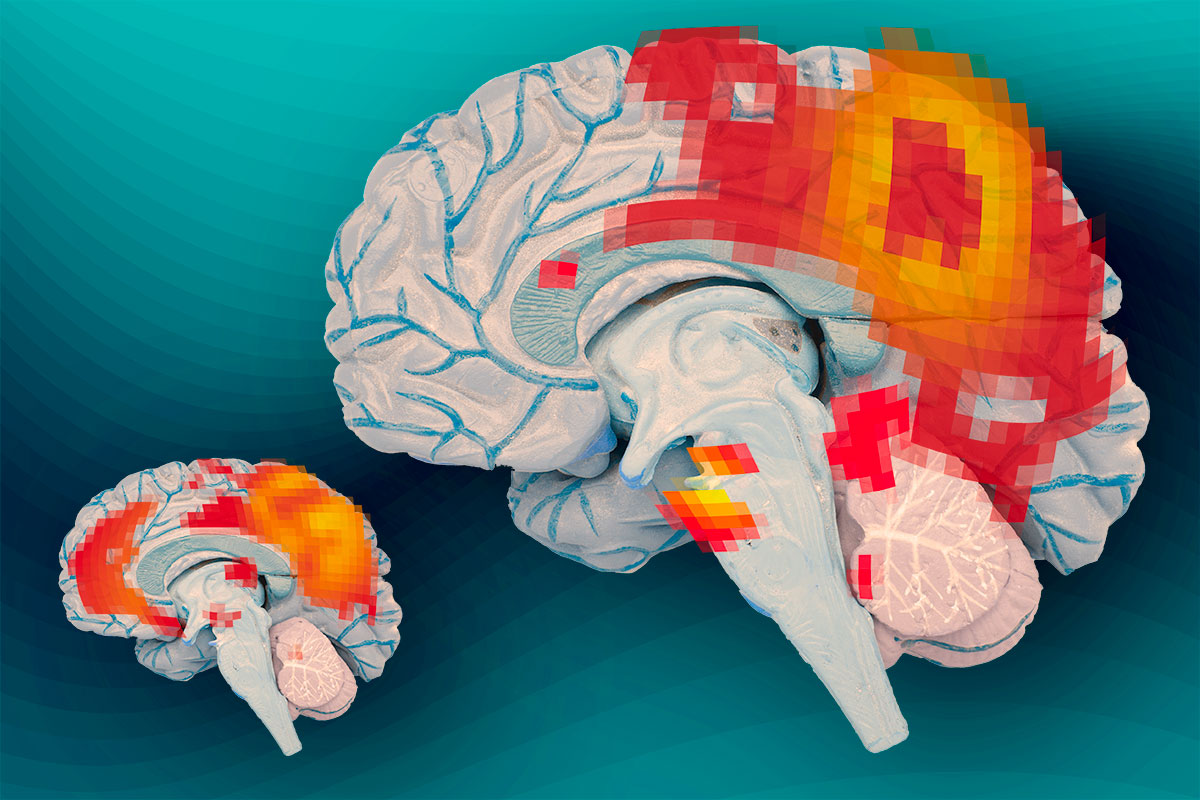
At left, the brains of adults who had ADHD as children but no longer have it show synchronous activity between the posterior cingulate cortex (the larger red region) and the medial prefrontal cortex (smaller red region). At right, the brains of adults who continue to experience ADHD do not show this synchronous activity.
Illustration: Jose-Luis Olivares/MIT (based on images courtesy of the researchers)
According to the CDC, as of 2011, approximately 11 percent of children ages 4 to 17 have been diagnosed with attention deficit hyperactivity disorder (ADHD) in the U.S. While many eventually “outgrow” the disorder, some carry their difficulties into adulthood. About 10 million American adults are currently diagnosed with ADHD.
In a new study in the June 10 issue of the journal, Brain, MIT researchers compared patterns of brain activity in adults who had ADHD as children but do not have the disorder as adults, and those who still have the disorder. This is the first study of its kind, and MIT neuroscientists have discovered key differences in a brain communication network that is active when the brain is at wakeful rest and not focused on a particular task.
According to the researchers, these findings offer evidence of a biological basis for adult ADHD and could help better diagnose the disorder.
This study focused on 35 adults who were diagnosed with ADHD as children; 13 still have the disorder as adults, while the others no longer have ADHD. “This sample really gave us a unique opportunity to ask questions about whether or not the brain basis of ADHD is similar in the remitted-ADHD and persistent-ADHD cohorts,” says Aaron Mattfeld, a postdoc at MIT’s McGovern Institute for Brain Research and the paper’s lead author.
The researchers used a technique called resting-state functional magnetic resonance imaging (fMRI) to study what the brain is doing when a person is not engaged in any particular activity. These patterns reveal which parts of the brain communicate with each other during this type of wakeful rest.
“It’s a different way of using functional brain imaging to investigate brain networks,” says Susan Whitfield-Gabrieli, a research scientist at the McGovern Institute and the senior author of the paper. “Here we have subjects just lying in the scanner. This method reveals the intrinsic functional architecture of the human brain without invoking any specific task.”
According to researchers at MIT, in people without ADHD, when the mind is unfocused, there is a distinctive synchrony of activity in brain regions known as the default mode network. Previous studies have shown that in children and adults with ADHD, two major hubs of this network — the posterior cingulate cortex and the medial prefrontal cortex — no longer synchronize.
In the new study, the MIT team showed for the first time that in adults who had been diagnosed with ADHD as children but no longer have it, this normal synchrony pattern is restored. “Their brains now look like those of people who never had ADHD,” Mattfeld says.
However, in another measure of brain synchrony, the researchers found much more similarity between both groups of ADHD patients:
In people without ADHD, when the default mode network is active, another network, called the task positive network, is suppressed. When the brain is performing tasks that require focus, the task positive network takes over and suppresses the default mode network. If this reciprocal relationship degrades, the ability to focus declines.
Both groups of adult ADHD patients, including those who had recovered, showed patterns of simultaneous activation of both networks. This is thought to be a sign of impairment in executive function — the management of cognitive tasks — that is separate from ADHD, but occurs in about half of ADHD patients. All of the ADHD patients in this study performed poorly on tests of executive function. “Once you have executive function problems, they seem to hang in there,” says John Gabrieli, professor of brain and cognitive sciences at MIT, and an author of the study.
Armed with this new information, reps for MIT say that the next step to “investigate how ADHD medications influence the brain’s default mode network, in hopes that this might allow them to predict which drugs will work best for individual patients. Currently, about 60 percent of patients respond well to the first drug they receive.”
“It’s unknown what’s different about the other 40 percent or so who don’t respond very much,” Gabrieli says. “We’re pretty excited about the possibility that some brain measurement would tell us which child or adult is most likely to benefit from a treatment.”


