Harvard Created an Artificial Spleen that Cleanses Blood
When a patient is diagnosed with sepsis, the life-threatening condition in which bacteria or fungi multiply in a person’s blood, it’s often too late for antibiotics to help. But, fortunately, Harvard researchers have developed a new device that transforms the way doctors treat sepsis and other blood infections.
A team of scientists from Wyss Institute for Biology Inspired Engineering created an artificial spleen called the Biospleen. The Biospleen quickens sepsis treatment by removing pathogens and toxins from a patient’s blood without having to identify the initial infectious agent.
Sepsis occurs when a patient’s immune system overreacts to a bloodstream infection, triggering a chain reaction that can cause inflammation, blood clotting, organ damage, and even death. It can arise from a variety of infections, including appendicitis, urinary tract infections, skin or lung infections, as well as contaminated IV lines, surgical sites, and catheters. Sepsis infects 18 million people worldwide and has a 30 to 50 percent mortality rate.
“Even with the best current treatments, sepsis patients are dying in intensive care units at least 30 percent of the time,” said Michael Super, senior staff scientist at the Wyss Institute, in a statement. “We need a new approach.”
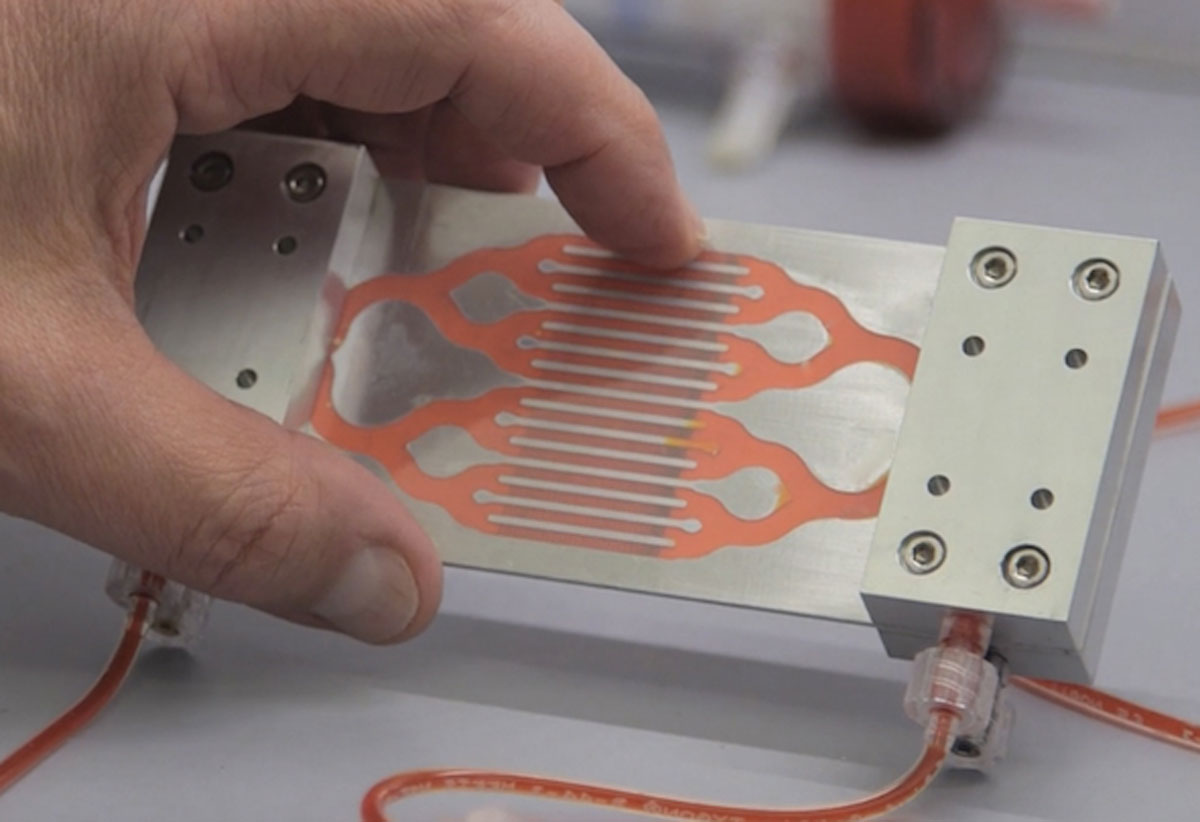
That new approach, says Donald Ingber, the Wyss Institute’s founding director, could be the Biospleen. It works like a dialysis machine: Blood is cycled outside of the patient’s body and filtered through microfluidic channels; the channels have nanoscale-sized magnetic beads that are coated with a genetically engineered human blood protein called mannose-binding lectin; the protein naturally latches onto bacteria, fungi, viruses, and toxins, and the magnets pull the magnetic beads out of the blood, taking the attached pathogens and toxins with them; lastly, the cleansed blood flows back into the patient.
“Sepsis is a major medical threat, which is increasing because of antibiotic resistance,” Ingber says. “We’re excited by the Biospleen because it potentially provides a way to treat patients quickly without having to wait days to identify the source of infection, and it works equally well with antibiotic-resistant organisms.”
During development, researchers tested the Biospleen by cleaning human blood that was spiked with different pathogens. When the blood flowed through the device, more than 90 percent of the pathogens were removed. The device was also tested on rats that had been infected by toxins and viruses such as E. coli and S. aureus. After just a few hours of filtering, 90 percent of the toxins and pathogens had been removed from the rats bloodstream, and 90 percent of the treated rats survived.
However, don’t expect the Biospleen to be used in hospitals anytime soon.
“We are currently advancing the technology to large animal validation studies, which we must complete successfully before applying for permission to move to human clinical trials,” Ingber says. “So the timing is unknown. But at least two years before trials would begin if we are successful.”
As for the future, the Biospleen could be used to treat patients suffering from viral diseases such as HIV and Ebola. In those cases, a person’s survival depends on how quickly the amount of virus in the blood can be lowered to a small enough level.