MIT Researcher’s Invention Could Save 1.8 Million Newborn Lives
About 1.8 million newborn babies die the day they are born each year because they have trouble breathing, mostly in low and middle-income countries, according to a study conducted by local doctors for BMC Public Health. Kevin Cedrone, an MIT post-doctoral researcher, hopes to lower that number with a prototype that will monitor a baby’s breathing after birth.
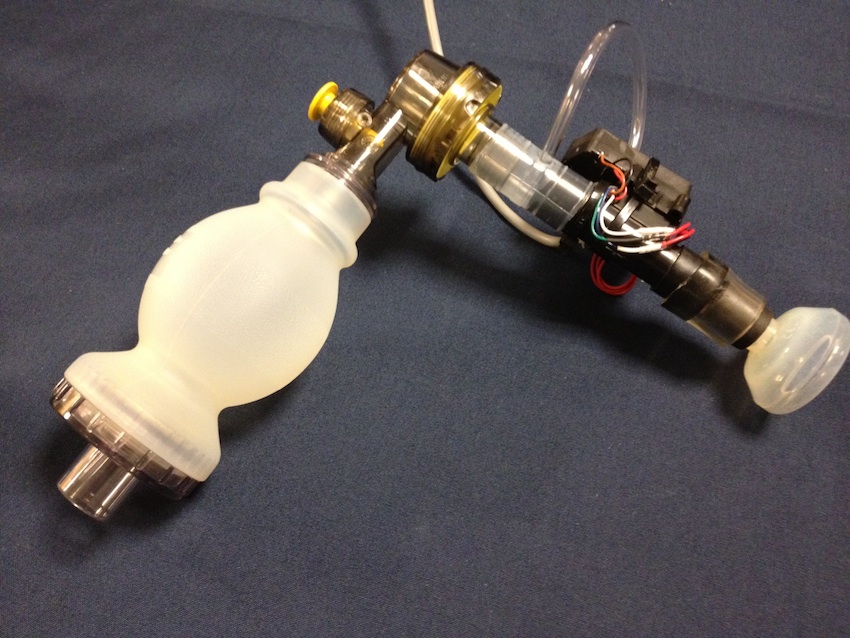
As a student at MIT, Cedrone built his prototype from spare lab parts in just one night. During a Massachusetts General Hospital hackathon, he collaborated with Dr. Santorino Data, a pediatrician in Uganda. Data brought up the fact that many babies were dying unnecessarily due to breathing problems after birth. “The problem seemed solvable to me,” Cedrone says. “So I wanted to collect data about why those deaths were occurring. We figured out that with unsophisticated, inexpensive sensors, we could give people real time feedback about resuscitation, and we could also help with training.”
Cedrone, who has a background in automotive engineering, realized that he had just thrown some sensors that would work for the project into the trash in his lab. So he took them out of the trash the next morning and made a mock device to prove to the board at the hackathon that he had a strong concept. The sensor would monitor an individual as he or she administered breathing to a dying baby, instructing them about the right pace, right amount of air, and right pressure that is necessary for saving a life. Cedrone and his collaborators won first prize at the convention.
Since the device’s conception, Cedrone and his team, which includes Craig Mielcarz of MIT, Dr. Data, and Dr. Kristian Olson of Massachusetts General Hospital, have won thousands of dollars in grants to develop the Augmented Infant Resuscitator (AIR) further. They recently won the IDEAS Global Challenge award and were given a $250,000 grant from the Saving Lives at Birth partnership. This grant will help the team to test the AIR prototype further, and Cedrone later hopes to bring the materials to hospitals for clinical trials.
“The plan is to build a few prototypes, take them to Uganda, and test them out,” Cedrone says. “It’s one thing to make a device that works, but it’s another to have people trust that device, ask for it, pay for it, and use it. We need the people in the clinics of Uganda to help with the development, design, and construction of this. We’ll hopefully be doing field trials early next year.”
Cedrone finds it ironic that although he’s doing his post-doc research in natural gas, and although his background is in automotive engineering, he’s been able to help solve medical problems. “It’s a departure from everything else I’m studying,” he says. “But partnerships with doctors make sense.” In general, Cedrone is able to solve problems fairly easily, as with this device, but he often doesn’t know what problems need to be solved in the medical world. He says that many doctors don’t know how to solve big problems, but they are aware of the problems that need to be focused upon. This partnership has been key for creating an innovative device that could save millions of lives.